8 Ways to Protect Yourself from Superbugs
Bacteria with a resistance to antibiotics are a real and present danger—especially for older adults. Here’s what you need to know to stay safe.
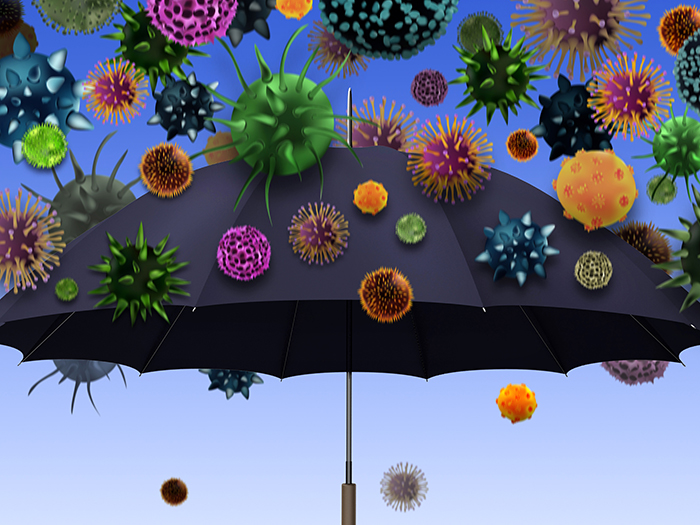
Superbugs. Sounds like something out of a science fiction novel. Unfortunately, when it comes to public health, superbugs are all too real.
It’s the common term for germs—including bacteria, viruses, fungi, or parasites—that develop resistance to the drugs used to treat them. Without a means to fight these germs, you can become very ill and spread the germs to others.
“Superbugs develop when you expose normal pathogens, or bugs, to a lot of antibiotics. Then they flip from sensitive to resistant organisms,” explains Lona Mody, M.D., M.Sc., a professor of internal medicine and associate division chief of geriatric and palliative care medicine at University of Michigan Medicine.
Antibiotic-resistant germs are being fueled by the decades-long antibiotic misuse and overuse in people, livestock, and agriculture.
Superbugs are one of the biggest public health threats in the United States today, says Lance Price, Ph.D., a professor at George Washington University Milken Institute School of Public Health and founding director of the Antibiotic Resistance Action Center (ARAC).
Each year 2.8 million antibiotic-resistant infections occur in the United States, resulting in more than 35,000 deaths, according to a new report from the Centers for Disease Control and Prevention (CDC).
And here’s the kicker: Older adults are more vulnerable to superbugs than younger people, thanks to the toll aging takes on the immune system and the fact that many of us spend more time in medical facilities, which can be a breeding ground for infections, as we get older.
Luckily, there are steps you can take to reduce your risk, whatever your age. But first, it’s important to know what you’re up against.
Seniors and Superbugs: Your Risk Factors
Many types of germs actually live on our skin, such as staphylococcus aureus (staph), or in our mouth, throat, gut, and vagina, such as the candida yeast.
In healthy people, these germs are usually harmless. If they grow out of control or become drug-resistant, that’s when they can turn against us.
Certain populations face a higher risk from superbugs:
- Older adults
- People who smoke
- Individuals with weakened immune systems
- Anyone with a chronic or underlying medical condition
- Those undergoing an invasive medical procedure, such as a surgery
- Hospitalized patients and those in long-term care settings
One of the biggest reasons seniors face a higher risk from superbugs is that the immune system degrades with age, says Price. But other reasons contribute, too.
“You start to have more overhaul-type surgeries, like hip replacement,” says Price. “As soon as you’ve cut the skin, you’re immediately at risk for infection.”
As we enter our 60s and 70s, our risk of blood infections also increases, with a 10-fold increase in men and four-fold increase in women, says Price. These are often the result of bladder or urinary tract infections (UTIs).
“UTIs are a major gateway for bacteria getting into the bloodstream, and that can be deadly,” says Price. “We are used to thinking of UTIs as a woman’s issue, but as we enter our 60s and 70s, the rates converge. Men and women start to get them at the same rate.”
In her research laboratory, Dr. Mody studies antimicrobial-resistant pathogens and measures to prevent them. In one study, she found one in four seniors brings germs from hospitals to post-care facilities, which many enter for rehabilitation.
Sloppy hand hygiene on the part of staff, patients, and visitors is the biggest culprit, says Dr. Mody. As a result, these germs can multiply and pose a risk to both the patient and other residents.
8 Ways to Safeguard Yourself Against Superbugs
The good news: There are steps you can take to protect yourself against drug-resistant germs.
1. Wash Your Hands Religiously
You’ve heard this before, but it’s one of the best ways to avoid getting sick, eliminate germs, and prevent them from spreading. Follow the CDC’s Clean Hands Count rules for any home care you are receiving or giving.
2. Get Vaccinated
Vaccines help prevent infections, such as pneumonia. “If you prevent any infection, there’s less chance to be exposed to antibiotics and therefore less chance to develop superbugs,” says Dr. Mody. You’ll also be less likely to be hospitalized with an infection, further reducing your exposure to antibiotics.
3. Use Antibiotics Wisely
Antibiotics treat only bacterial infections, such as strep throat or pneumonia. In some cases, they may be prescribed before surgery to reduce the risk of infection. Antibiotics don’t work on viral infections, such as the common cold or flu.
“If we take antibiotics when they aren’t called for, it can change our gut flora, increasing our risk of antibiotic-resistant infections,” says Dr. Mody.
If your doctor prescribes antibiotics, ask them if you really need it or if there are other ways to treat your illness, says Price. An estimated 30 percent of antibiotics prescribed or used in outpatient or hospital settings are unnecessary, reports the CDC.
4. Prevent UTIs
“Bladder health becomes really important as we get older,” says Price. Improper bathroom hygiene can spread bacteria, such as E. coli, that can cause UTIs. E. coli is another germ that is quickly becoming resistant to antibiotics.
Subscribe to our newsletter
It's quick and easy. You could be one of the 13 million people who are eligible.
Already a member? Click to discover our 15,000+ participating locations.
Follow Us
“Make sure you are drinking enough water and urinating frequently to prevent bacteria from growing,” says Price. “And wipe from front to back.”
5. Research Medical Facilities
Each year, more than a million infections are acquired in hospitals and other medical settings. Forty-four percent of these patients are age 65 or older. You can see how your local hospitals compare to the national average at medicare.gov.
6. Speak Up for Better Care
When you’re sick or hospitalized, it’s important to make sure everyone around you washes their hands. According to the CDC, on average, providers clean their hands less than half of the times they should.
“Patients should feel comfortable asking the nurse to wash their hands. Or ask the doctor, if they haven’t seen them do it,” says Dr. Mody.
7. Research Overseas Travel
“Some countries have very high rates of extremely resistant bacteria,” says Price. The most common travel-related illness, traveler’s diarrhea, can also be drug-resistant.
Destinations at the highest risk are in Asia (except for Japan and South Korea), as well as Mexico, Africa, the Middle East, and Central and South America.
8. Reconsider Medical Tourism
To save money, you may have considered having an elective surgery or medical procedure overseas. You might want to think again: One serious emerging public health threat in the United States is candida auris, a potentially fatal fungal infection that’s resistant to multiple antifungal drugs. C. auris can live on surfaces for weeks, making it difficult to contain.
Of the more than 800 cases in the United States, the majority were diagnosed in New York City, New Jersey, and Chicago—but that’s not where the infections started. Most originated abroad, after a patient received care in a country where C. auris had been reported.
Remember, even if you’re fit and healthy, superbugs you carry can get others sick. “When we practice good hygiene and take other precautions, we are curbing germs and infections that could be harmful to people who don’t have adequate immunity to fight those infections,” says Dr. Mody.
Take Your Favorite SilverSneakers Classes Online!
SilverSneakers members can access live fitness classes and wellness workshops through SilverSneakers LIVE. See the latest schedule and RSVP for classes here.
Not a member? If you have a Medicare Plan, it may include SilverSneakers—at no additional cost. Check your eligibility instantly here.




